Diagnostic Errors: A Persistent Risk
- -
By Laura M. Cascella, MA
The term “medical error” often conjures thoughts of wrong site surgeries, procedures performed on the wrong patients, foreign objects left inside patients, medication mistakes, and other serious mishaps.
Although these errors certainly deserve attention, the visibility surrounding them can easily overshadow common, but less sensational lapses. Diagnostic errors, for example, “commonly occur with dire human and economic consequences.”1 Although these errors have sometimes taken a backseat in national patient safety efforts, they have been a long-standing medical malpractice concern.
Over the years, MedPro Group has monitored and analyzed diagnosis-related claims to better understand how and why diagnostic errors occur and to develop comprehensive risk education for insureds. This article provides an overview of the issues surrounding diagnostic errors and examines detailed data that show how these errors contribute to malpractice allegations and claims.
The Scope of the Problem
Diagnostic errors occur at an “appreciable, though unknown, rate.”3 Some estimates suggest that the diagnostic error rate is in the range of 10–15 percent, with variations across specialties.4 Further, the authors of a 2011 study about ways to reduce diagnostic errors note that errors associated with diagnosis are more likely to be preventable and more likely to result in patient harm than other types of medical errors.5
Yet, if diagnostic errors represent such a significant burden, why are they so often the wallflowers of patient safety and quality initiatives? Although it’s difficult to find a definitive reason, a number of factors might be at play. For example, diagnostic errors may receive inadequate attention because (a) they often go unrecognized or unreported, (b) they can be difficult to understand and measure, and (c) they don’t always have clear-cut solutions.6
In the last decade, however, various circumstances have pushed diagnostic errors closer to the limelight. A 2013 article about diagnostic error detection lists the following reasons for the increased attention:
- New models of care delivery, such as accountable care organizations, that reward clinicians for correct diagnoses
- Greater focus and financial support as a result of the formation of the Society to Improve Diagnosis in Medicine
- Advocacy on the part of the American Medical Association’s Center for Patient Safety
- High-profile cases, such as a child who died of septic shock after being diagnosed with a minor stomachache
- Health information technology (HIT) opportunities, including alerts and alarms built into electronic health record systems
- Increasing emphasis on team decision-making, particularly for rare and serious conditions7
Although these factors represent important strides, recent literature focusing on diagnostic errors notes the need for additional research to identify gaps in the diagnostic process and study various risk-reduction techniques.
Learning From Malpractice Claims Data
Despite a historic lack of attention, diagnostic errors result in a higher frequency of malpractice claims (for physicians) and larger average indemnities than other types of allegations (for both physicians and dentists).8
A 2013 Medscape article explains that “although malpractice claims may not be a representative measure of adverse events [related to diagnostic errors], they can provide insight into the types and sources of adverse events.”9
With this in mind, the following data from the National Practitioner Data Bank (NPDB) and MedPro Group* help illustrate the impact of diagnostic errors on both the medical and dental communities.
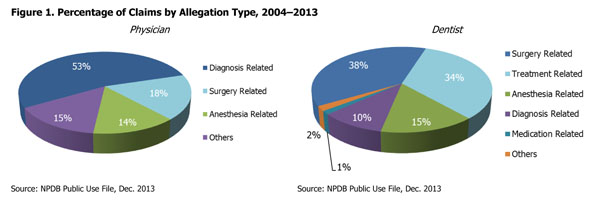
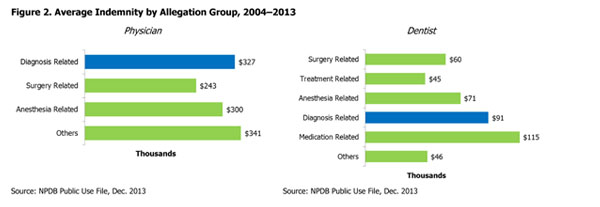
Data from the NPDB show that diagnosis-related allegations represent more than half of all physician claims. For dentists, diagnosis-related allegations represent 1 in 10 claims; however, they are second in average indemnity, trailing only medication-related allegations (see Figures 1 and 2). For both physicians and dentists, the top allegation category within diagnostic allegations is failure to diagnose.10
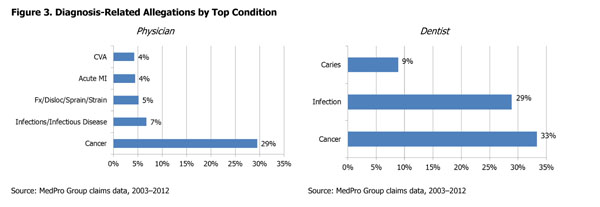
Analysis of MedPro Group’s diagnosis-related claims opened between 2003 and 2012 reveals that, for both physicians and dentists, cancer is the condition most frequently associated with these claims (see Figure 3).
For physicians, the top five types of cancer in diagnosis-related allegations are lung/trachea, colorectal, breast, lymphatic/hematopoietic, and prostate. Cancers of the tongue account for one-third of cancer-related dental claims, followed by cancers of the gums and cheeks.
(Note: These rankings are related to the data source noted, and may vary across data sources.)
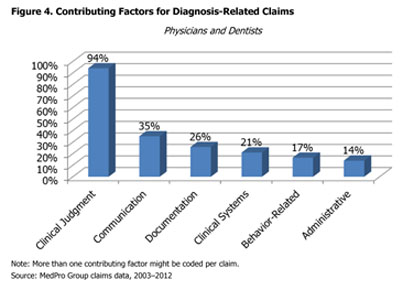
Various factors can contribute to diagnostic allegations (see Figure 4). Contributing factors are broad areas of concern that may play a role in allegations, injuries, or initiation of claims. For both physicians and dentists, clinical judgment is the leading factor, occurring (with some variability) in the majority of claims.
Within these broad areas of concern are more specific issues that may lead to diagnostic mishaps or failures. Examples of such issues include:
- Vulnerabilities in clinical workflow processes and organizational policies
- Cognitive failures or biases
- Breakdowns in interaction between systems and providers
- Issues with information synthesis
Claims may involve multiple issues and contributing factors, as well as more than one provider. In fact, many diagnosis-related claims are multifactorial.11 Hence, in a 2013 research article about the type and origins of diagnostic errors, the authors explain that strategies to address diagnostic errors should “account for their common contributory factors and not just attempt to augment knowledge or clinical skills related to specific diseases because such interventions may not generalize across diseases or care settings.”12
From a risk management perspective, contributing factors are important because they might be amenable to risk-reduction strategies. Identifying the factors that drive claims and taking corrective actions to address them are key risk management strategies.
Conclusion
Diagnostic errors represent a frequent, serious, and costly risk. Although not all diagnostic errors result in adverse events, many do — creating legitimate patient safety and liability concerns.
Endnotes
* MedPro Group has entered into a partnership with CRICO Strategies, a division of the Risk Management Foundation of the Harvard Medical Institutions. Using CRICO’s sophisticated coding taxonomy to code claims data, MedPro Group is better able to identify clinical areas of risk vulnerability. All subsequent data attributed to MedPro Group represent a snapshot of MedPro Group’s experience with diagnosis-related claims, including a deep dive into risk factors that drive the claims.
1 McDonald, K. M., Bryce, C. L., & Graber, M. L. (2013, October). The patient is in: Patient involvement strategies for diagnostic error mitigation. BMJ Quality and Safety, 22(Suppl 2), ii33–39.
2 Phua, D. H., & Tan, N. C. (2013). Cognitive aspect of diagnostic errors. Annals of the Academy of Medicine, Singapore, 42(1), 33–41.
3 Ely, J. W., Graber, M. L., & Crosskerry, P. (2011, March). Checklists to reduce diagnostic errors. Academic Medicine, 86(3), 307–313.
4 Crosskerry, P. (2013, June). From mindless to mindful practice — cognitive bias and clinical decision making. New England Journal of Medicine, 368(26), 2445–2448.
5 Ely, et al., Checklists to reduce diagnostic errors.
6 Zwaan, L., Schiff, G. D., & Singh, H. (2013, August). Advancing the research agenda. BMJ Quality and Safety, 22(Suppl 2), ii52–57; Graber, M. L., Wachter, R. M., & Cassel, C. K. (2012). Bringing diagnosis into the quality and safety equations. Journal of the American Medical Association, 308(12), 1211–1212.
7 Clark, C. (2013, November 7). Diagnostic error detection comes into focus. HealthLeaders Media. Retrieved from http://www.healthleadersmedia.com/page-1/QUA-298106/Diagnostic-Error-Detection-Comes-Into-Focus
8 National Practitioner Data Bank Public Use File, Dec. 2013.
9 Brown, T. (2013, July 18). Missed diagnoses may trigger primary care malpractice claims. Medscape. Retrieved from http://www.medscape.com/viewarticle/808132
10 National Practitioner Data Bank, Public Use File, December 2013.
11 Wallace, E., Lowry, J., Smith, S. M., & Fahey, T. (2013, July). The epidemiology of malpractice claims in primary care: A systematic review. BMJ Open, 3(7), 1–8.
12 Singh, H., Giardina, T. D., Meyer, A. N., Forjuoh, S. M., Reis, M. D., & Thomas, E. J. (2013, March 25). Types and origins of diagnostic errors in primary care settings. Journal of the American Medical Association Internal Medicine, 173(6), 418–425.
The information provided in this document should not be construed as medical or legal advice. Because the facts applicable to your situation may vary, or the regulations applicable in your jurisdiction may be different, please contact your attorney or other professional advisors if you have any questions related to your legal or medical obligations or rights, state or federal statutes, contract interpretation, or legal questions.
The Medical Protective Company and Princeton Insurance Company patient safety and risk consultants provide risk management services on behalf of MedPro Group members, including The Medical Protective Company, Princeton Insurance Company, and MedPro RRG Risk Retention Group.
© MedPro Group.® All Rights Reserved.
